General medicine case history 1
74. S.Nithesh
GM Case history-1
August 10, 2021
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
Date of admission: 09-08-2021
A 56- year- old woman presented to the OPD with chief complaints of fever, decreased urine output since 3 months and breathlessness from the past 3 days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 5 years back, then had fever which was insidious and associated with chills, vomiting and pain in the loin for which she went to outside hospital where she was diagnosed with kidney disease, from then she was on medication.
7 months back she stopped medication for 1 month, then after that she developed shortness of breath for which she went to a local hospital where she was referred to our hospital.
She was diagnosed to have chronic kidney disease and adviced to get hemodialysis done
From then on she was on hemodialysis twice weekly.
Now for the past 3 days she is complaining of high grade fever which was associated with chills and rigors and nausea , vomiting of 2 episodes non billions, non projectile, food as content
Not associated with pain abdomen or loose stools.
PAST HISTORY:
K/c/o Hypertension since 6 years
Not a known case of CAD, Asthma,TB, Epilepsy, Thyroid disorders.
No history of sugeries and blood transfusions in the past.
PERSONAL HISTORY:
The patient is a vegetarian.
Appetite is decreased due to dialysis
Regular bowel and bladder movements
Normal sleep
No addictions
FAMILY HISTORY:
There are similar complaints in the family( The patient's mother and sister had suffered from the similar condition).
No cancer deaths in the family.
TREATMENT HISTORY:
The patient is not allergic to any known drugs.
GENERAL EXAMINATION:
On examination,the patient is conscious, coherent, co-operative.
No icterus and pedal edema.
The patient has pallor
No cyanosis, clubbing, edema, lymphadenopathy.
VITALS:
Temperature-98⁰F
Pulse rate-118bpm
Respiratory rate-18 cpm
BP - 100/50 mm/Hg
SPO2 at room air-98%
GRBS- 127 mg/dl
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
S1 and S2 sounds heard, no murmurs.
RESPIRATORY SYSTEM:
Position of trachea- central
Dyspnoea- present
Normal vesicular breath sounds heard
No wheezing
No additional sounds heard.
PER ABDOMEN:
Abdomen is soft and non tender.
Bowel sounds heard.
No palpable mass or free fluid.
CENTRAL NERVOUS SYSTEM:
The patient is conscious
Speech: normal
No signs of meningeal irritation
Motor and sensory system: normal
Reflexes- present
Cranial nerves- intact.
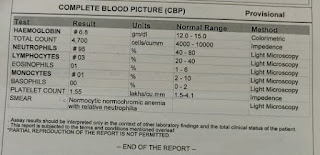
INVESTIGATIONS:
09-08-2021:
PROVISIONAL DIAGNOSIS:
Chronic kidney disease?
FINAL DIAGNOSIS:
Chronic kidney disease with k/c/o hypertension
TREATMENT :
- Fluid (<2L/day) and salt restriction (<2gm/day)
- TAB. LASIX 40mg PO BD
- TAB. PCM 500mg PO
- TAB. OROFER- XT PO OD
- TAB. SHELCAL 500mg PO OD
- TAB. NODOSIS 500 mg PO OD
- TAB. NICARDIA 10mg PO BD
- BP and fever charting, inform SOS.
Archive
Report Abuse






Comments
Post a Comment